
By Bill Rice Jr.
- Husband and wife have both tested positive for antibodies
- First symptoms emerged in mid-December - 2 weeks before Wuhan outbreak
- Tim McCain, who almost died, would have been first CV-19 fatality in world
- Story has received no national attention
- Couple - possible “Patients Zero” in U.S. - has yet to be contacted by health officials
- Wife never left hospital, saw first-hand the ‘nightmare’ critical COVID patients endure
- Hospital staffers who treated McCain will not comment on his case
- Director of nursing previously expressed opinion Tim McCain ‘definitely” had COVID-19
- Couple believes lessons from husband’s case could have saved lives
- Medical bill exceeds $2 million
- ECMO machine credited with saving husband’s life; possibly first case in world
- Medical records support COVID-19 diagnosis
On January 4, Tim McCain - a 38-year-old father of two from Sylacauga, Alabama - nearly lost his life in a medical drama that began in late December.
“It’s a miracle he survived,” says McCain’s wife, Brandie McCain, 39.
Her husband did survive, but if he had not Tim McCain might today be considered the first COVID-19 fatality in the world.
 Tim McCain (Photo courtesy of Brandie McCain)
Tim McCain (Photo courtesy of Brandie McCain)
At the moment, a 61-year-old man from Wuhan, China - who died January 9th, five days after Tim McCain’s near-death experience - is considered the world’s first known COVID-19 fatality. Patricia Dowd, a 57-year-old California woman who passed away February 6th, is considered America’s first known COVID-19 death. Mrs. Dowd’s death occurred 33 days after Tim McCain was admitted to the Cardiac Intensive Care Unit at Grandview Medical Center in Birmingham, Alabama in critical condition.
Both McCains believe Tim nearly died after experiencing an extreme medical reaction triggered by the novel coronavirus. Evidence supporting the belief Tim McCain had COVID-19 in December is convincing.
First, both McCains have tested positive for COVID-19 antibodies (from the Abbott IgG assay).
Second, both of the McCains experienced virtually all of the COVID-19 symptoms, including more unique symptoms typically associated with COVID-19. In addition to Tim and Brandie McCain, at least four other people in the couple’s immediate circle of daily contacts also developed symptoms typical of those who have tested positive for COVID-19.
Third, numerous details of Tim’s clinical case history mirror those of COVID-19 ICU patients in Wuhan China (here and here) and later in the United States.
Four, according to Brandie McCain, many of those who cared for Tim soon came to believe Tim’s severe illness was indeed caused by COVID-19.
Until last month, the Alabama couple believed they might be the first confirmed, or likely, COVID-19 patients in the country. However, stories in The Seattle Times and The Palm Beach Post have identified at least 13 other people who had COVID-19 symptoms as early as November and December. Like the McCains, all 13 tested positive for COVID-19 antibodies. But none of these individuals came close to dying.
Hospital quarantine policies enacted six weeks after Tim was discharged from the Birmingham hospital preclude family members of COVID-19 patients from being with their loved ones. Because of this, Brandie McCain is perhaps the only family member of a critical COVID-19 patient in the United States who witnessed the “sheer hell” such patients endure.
Today, however, she’s “torn” about whether these loved ones would actually want to live
through the “nightmare” she and her family experienced.
“I know what they would see,” says Brandie, who never left the hospital during her husband’s 24-day hospital stay. “It is bad … It is bad.”
The McCains are also bewildered they’ve yet to be contacted by a single state or national
health care official seeking information regarding the circumstances of their cases, including information on how and when they may have contracted the novel coronavirus and who else they may have infected.
“You would think that someone would be testing us for antibodies every week if for no other reason than to see how long these antibodies last,” says Brandie.
CDC officials have pushed back the date when “limited community transmission” of SARSCoV-2 may have begun in this country. However, this new timeline begins at least one month after Tim and Brandie McCain report the onset of their first COVID-19 symptoms.
According to an announcement made May 29th at the CDC’s first press briefing in two months, “Information from diverse data sources (now) suggests that limited community transmission of SARS-CoV-2 in the United States occurred between the latter half of January and the beginning of February,” reported NBC News.
“There was no indication the virus had been introduced into the U.S. earlier, in November or December. We looked for evidence of early widespread transmission and could not confirm it,” Dr. Jay Butler, deputy director for infectious diseases at the CDC, said. He added his team will continue to search for clues of the first cases on U.S. soil.
According to Brandie McCain, no person “search(ing) for clues of the first cases on U.S. soil” has contacted the McCains, who might qualify as “Patients Zero” in the nation. At least one of Tim’s care-givers at Grandview Medical Center told the couple to expect such a follow-up from epidemiologists, “which never happened,” says Brandie.
She also says at least one person who treated Tim McCain told the couple they should contact the Red Cross to donate samples of their blood plasma (which are needed for COVID-19 research). This alleged conversation would also indicate that another Grandview Medical Center staffer believed the McCains either did, or might have had, COVID-19 in December.
Brandie McCain says she’s remained in contact with several individuals who provided medical care to her husband at Grandview Medical Center in January. According to Brandie, by mid or late February, she’d spoken with these individuals about the possibility Tim might have had COVID-19. “Everyone” she talked to shared the opinion that Tim almost certainly did have COVID-19, says Brandie.
After Brandie made a post on her Facebook page announcing that the couple’s antibody tests had come back positive, Jordan Pugh, the director of Grandview Medical Center’s CICU nursing unit, replied in a personal message:
“I knew it would!!!! He definitely had it and we had no idea!!”
This reporter requested interviews with individuals who were involved in Tim McCain’s care at Grandview Medical Center. A week after making this initial request, hospital spokesperson Leisha Harris replied via a text message.
“I do not have anyone interested in being interviewed,” the text said.
Ms. Harris has yet to reply to a follow-up email that included several questions including these:
“Has anyone at Grandview Medical Center forwarded details of Tim McCain’s case history to state or national health care officials who may be compiling data on known or likely CV-19 patients?”
“Did any hospital staffers (involved in Mr. McCain’s care in January) later contract COVID-19 or experience symptoms common to COVID-19 patients?”
Brandie and Tim McCain also believe lessons from Tim’s medical drama could have been used to save lives of other critical COVID-19 patients.
Months after Tim had returned home, Brandie received a link to an article that included a dispatch from an “anonymous” New Orleans emergency room physician who helped treat many critical COVID-19 patients in that city’s surge of COVID-19 patients in late March.
According to Brandie, The detailed observations of the physician - which included several warnings about treatments doctors should avoid - contained numerous similarities to Tim’s case. The similarities “blew me away,” she says. This reporter documented the parallels in this piece.
***
At approximately 3:25 a.m. on Saturday, January 4th, Tim McCain somehow managed to walk into Coosa Valley Medical Center in Sylacauga and tell emergency room personnel, “I can’t breathe.”
Within seconds, “everyone in the room” was moving in a blur, remembers his wife.
First, someone measured Tim’s blood oxygen levels.
The figure - 84 percent - would later fall “into the 70s,” says Brandie.
Remembers Tim: “The doctor told me I was basically dead and that I shouldn’t be sitting there talking to him.”
Medical personnel then performed an X-ray on Tim’s chest. The X-ray helped confirm Tim had bilateral pneumonia and was suffering from Acute Respiratory Distress Disorder (ARDS).
The image basically showed a mass of white, says Brandie. “You couldn’t even tell he had
lungs.”
Two hours later, Tim McCain was in an ambulance racing to Grandview Medical Center in Birmingham, 45 minutes away. A doctor told Brandie he wasn’t sure her husband would survive the trip. Brandie looked the doctor in the eyes.
“Yes, he will,” she said.
***
“Everybody keeps telling me it’s a miracle I am alive,” says Tim McCain, who also goes by Timmy.
Everybody is right.
“What he went through was horrible, a nightmare,” says his wife.
Within 24 hours of his arrival at the Birmingham hospital, Tim’s thoracic surgeon “called the family together” to prepare them for the worst.
According to Brandie, the surgeon told family members Tim needed an emergency operation to connect him to an ECMO machine, a device that draws blood out of a patient’s body, adds oxygen to it, and then pumps the oxygenated blood back into his heart. (While other critical COVID-19 patients have since been placed on the device, Tim is possibly the first COVID-19 patient in the world whose life was saved by ECMO.)
 Tim McCain in the ICU during his battle with what is now believed to be COVID-19
Tim McCain in the ICU during his battle with what is now believed to be COVID-19
While Tim survived the operation, his prognosis remained bleak. He spent the next two weeks in a medically-induced coma incubated on a ventilator and on the ECMO machine.
According to Tim’s wife, “a whole team of nurses” cared for her husband around the clock. He “coded” several times and had to be resuscitated in terrifying episodes, several of of which she and the couple’s two teenage children witnessed. Early in his stay, Tim went into sepsis, a potentially fatal condition that develops in more than half of critical COVID-19 patients, according to one medical study. In the span of three weeks, he was given 34 units of blood, and, in a time period of approximately four weeks, lost 80 pounds.
After 24 days in the hospital’s Cardiac Intensive Care Unit, Tim was discharged from Grandview on January 28th. By mid-February, he felt strong enough to return to work.
With the exception of a lingering cough, minor numbness in one leg and a few other small ailments, “I feel as good as I’ve felt in years,” says Tim.
***
Tim McCain began to feel feel as miserable as he’s felt in his life the day after Christmas, which was more than a week after Brandie McCain experienced her first COVID-19 symptom - persistent pain in her lower back, a common if perhaps under-reported complaint of patients diagnosed with COVID-19.
“I had awful back pain,” says Brandie, who first noticed this pain on or just before December 15th.
“A couple of days later,” her husband also developed serious pain in his lower back, pain severe enough to make him visit a local urgent care facility.
“It wasn’t like normal muscle pain,” says Tim. “It felt like it was in my bones. It was hurting the joints in my back.”
A physician at a local urgent care facility gave Tim a steroid shot and prescribed a “steroid pack” of pills, says Brandie. The McCains speculate that either the steroids and/or IV fluids Tim was given a couple days later may have triggered the severe negative reaction that almost caused his death.
The couples’ “flu-like symptoms” hit both of them the day after Christmas.
Tim thought he’d come down with “the regular flu … I thought I would get over it, but it kept getting worse and worse and worse.”
Brandie McCain also became “very sick” on December 26th.
“I couldn’t get out of bed for two days,” she says. Like her husband, she had symptoms
common to COVID patients, including a bad and persistent cough and the loss of smell and taste, two symptoms that persist even today. Tim also experienced a loss of smell and taste, which has since returned. The couple’s two teenage children became ill at the same time, but their symptoms were relatively mild (their daughter’s sense of smell and taste has also not returned, says Brandie).
At the time, family members were temporarily living at a friend’s house. The friend, Ben Calfee, said that he “was about as sick as I’ve ever been,” at the same time, adding, “there’s no doubt in my mind I had it (COVID-19) … I had all the symptoms that go with it.” Calfee has yet to receive an antibody test.
Brandie’s boss, Phil Cain, also developed flu-like symptoms around the first of January, as well as the worse back pain he’s ever experienced, he says. The pain - which started around his shoulders and later moved to his lower back - lasted about “two and a half months” before suddenly disappearing, he says. Cain says he has since tested negative for COVID-19 antibodies.
Tim McCain and Calfee spent New Year’s Eve watching TV, commiserating about their illness.
“I remember Ben saying, ‘Man, this is going to kill us,’ “ recalls Tim.
By 9 o’clock on the evening of New Years Day - five days after the onset of his flu-like
symptoms - Tim felt bad enough to go to the local emergency room.
While at the hospital, he was tested for influenza and came back positive. (Studies confirm that many COVID-19 patients have also tested positive for influenza. Brandie tested “negative” for influenza.) The fact Tim had Type A influenza and, likely, COVID-19 at the same time is another possibility that might explain Tim’s health crisis, Brandie speculated.
Tim was discharged after being given IV fluids and receiving a chest X-ray. However the scans were not immediately examined by a radiologist. Later the McCains did see the Jan. 1st X-rays. The contrast between the fairly normal images of Jan. 1st and the ones he received early in the morning of January 4th are stunning. Whatever attacked his lungs and chest happened very fast.
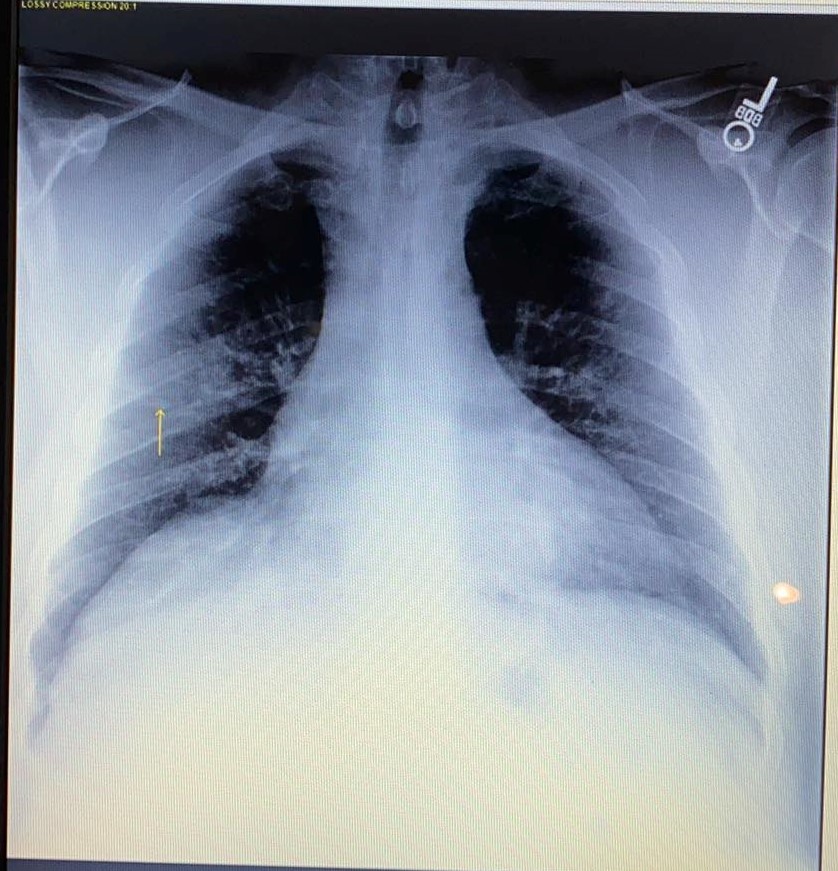 Tim McCain's chest X-Ray from 1/1/20
Tim McCain's chest X-Ray from 1/1/20
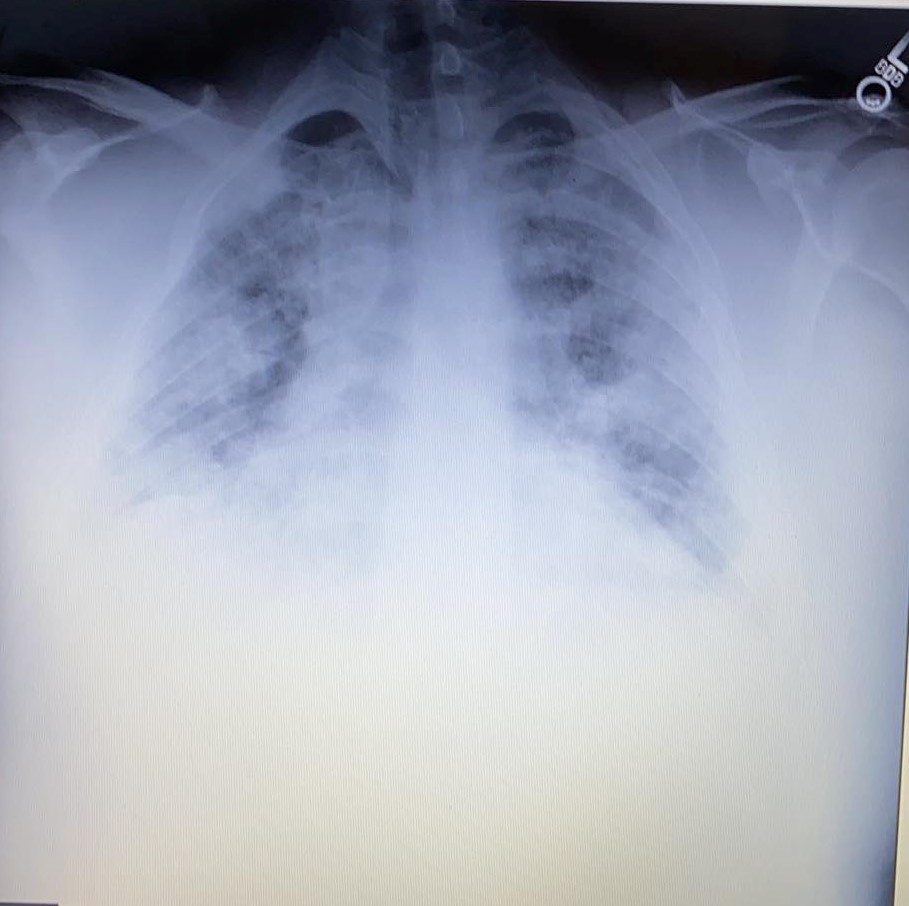 Tim McCain's chest X-Ray appx 54 hours later
Tim McCain's chest X-Ray appx 54 hours later
Over the ensuing three days, Tim’s symptoms rapidly worsened. His fever peaked at 104, he had “aches and pains over my entire body,” a bad cough, extreme fatigue and acute shortness of breath.
“I don’t think I ever walked more than 10 steps from my bed,” he says. “Getting out of bed and walking to the bathroom or the shower, I couldn’t do it.”
On Friday, January 3rd things became critical.
That evening Brandie helped Tim get to the bathroom. “He thought a bath would make him feel better,” says his wife. While he was in the bath, Brandie noticed her husband’s “color was not right. He looked yellow to me.” After Tim finished his bath, she helped him put on his clothes. “He couldn’t do it himself,” she says. His breathing was so “short and rapid … I thought he was going to pass out.”
By 3 a.m., it was clear Tim required immediate medical help. With Brandie’s help, Tim was able to make it to the car and his wife rushed him to the local hospital.
On January 16th, after 11 days on the ECMO machine, Tim’s Birmingham doctors removed him from the device. Almost immediately, he began to emerge from his medically-induced coma.
When Tim woke up, he was suffering from “ICU psychosis.” He says a prolonged dream he’d been having was incredibly realistic.
“I thought I was on a military hospital ship at Pearl Harbor,” he says. He was convinced his legs had been blown off while he was piloting a plane defending the naval base. “I even pulled the sheets down to show Brandie - ‘Look, I’ve got new legs. I can go back now,’ ” he said.
On January 19th, doctors took him off the ventilator and on January 28 he was back in
Sylacauga.
“It was amazing how fast (his condition) improved,” notes Brandie.
***
Three weeks after Tim was released from the hospital an outbreak of the novel coronavirus in Wuhan China was beginning to dominate global news reports.
“Everybody kept telling me I probably had it,” says Tim, who initially rejected this possibility.
“I was just working off what the doctors told me at that time,” he says, which was that he’d had some mysterious reaction to the “regular flu” which triggered his ARDS. At some point, however, he began to seriously entertain the idea that he may have contracted COVID-19. “I definitely had all the symptoms,” he says.
Brandie and Tim were eager to receive antibody tests as Brandie believed a positive result would mean her husband was now immune to COVID-19 (scientists believe this may be the case, although no definitive study has confirmed this to date). On April 30th Brandie received an email informing her that a local medical clinic was now offering a COVID-19 antibody test; the next day she was one of the first people in town to receive the test.
“When they called and told me I was positive, I knew that Tim’s test would be too,” she says. “I started crying … It was like a breath of fresh air because it gave me hope that maybe Timmy won’t ever get that sick again. If Timmy did not have COVID, and he got it now, I was going to lose my husband.
Tim felt the same way.
“I know my body wouldn’t be strong enough to fight off something like that again,” he says.
Both Brandie and Tim tested “positive” on the “IgG” serology assay created by Abbott, one of the most common antibody tests being used by medical practices throughout the country. According to language on lab reports, a positive IgG result “suggests recent or prior infection with SARS-CoV-2.” They both tested negative on the IgM test, which is typically positive when a person was infected more recently.
 Tim McCain's Positive Antibody Test Results
Tim McCain's Positive Antibody Test Results
 Brandie McCain's Positive Antibody Test Result
Brandie McCain's Positive Antibody Test Result
Both McCains are surprised their two teenage children tested “negative” for antibodies.
Brandie speculates that the children’s younger age, or the fact they experienced only mild symptoms might explain these results
“Maybe (COVID-19) antibodies remain in some people’s blood longer than other people?” says Brandie.
Mrs. McCain may be right. According to at least one recent study, COVID-19 antibodies seem to disappear in many confirmed COVID-19 patients in “just a few months.”
As Brandie experienced her first COVID-19 symptom (her “awful” back pain) on or near December 15 and the incubation period for the novel coronavirus is believed to be two to 14 days, Brandie McCain could have contracted COVID-19 as early as December 1st or as late as December 13th. This would be at least two weeks before the government in Wuhan, China, confirmed that health authorities were treating dozens of cases (on December 30th).
Recognizing the potential significance of the couple’s story, on May 6 Brandie contacted a
Birmingham TV station (Fox affiliate WBRC) via the station’s Facebook page. A reporter
responded almost immediately, says Brandie. On May 8th, the station aired a 90-second story.
Surprisingly, no other news organization in the country picked up the story, and no reporter except this one has followed up with the couple.
Both McCains believe that COVID-19 was circulating, perhaps widely, in their community and probably in many areas of the country, weeks or months before is commonly believed. They believe they probably contracted the novel coronavirus in their small central Alabama town (population 12,000), although it’s possible Tim contracted it in Montgomery where he
commutes to work. (Brandie and her sister did take a Caribbean cruise November 2-10 but Brandie believes the fact her first COVID-19 symptom didn’t emerge until December 15th - 35 days after the cruise - makes it unlikely she contracted the virus on this cruise).
Brandie added that “it seems like everybody in town” was experiencing flu-like symptoms in December and January.
Indeed, on April 5th, UncoverDC.com published an exclusive story that showed a spike in “influenza like illness” beginning in November in many states. As the article notes, the vast majority of patients complaining of COVID-19-like symptoms tested negative for influenza, a detail that leaves open the possibility that a certain percentage of these “flu-negative” sick people may have had COVID-19. A study published by researchers at Penn State University on June 22nd (“Initial COVID-19 infection rate may be 80 times greater than originally reported”) supports the hypothesis first presented by UncoverDC.com.
***
Nearly six months after Tim was admitted to the Birmingham hospital, Brandie still
experiences flashbacks to moments when her husband nearly died - times when he
experienced seizures and convulsions, when “blood was pouring out of the side of his mouth,” when doctors or nurses had to “bag” Timmy (force a mask on his mouth to pump oxygen into him).
“I’m sure I have PTSD,” she says today.
According to Brandie, the couple’s medical bills exceed $2 million of which the family’s
insurance policy covered only $900,000. To help satisfy this debt, the couple has already
forfeited Tim’s Harley Davidson motorcycle.
While Brandie knows they will never be able to pay off the bill, “I don’t care. Timmy is alive,” she says.
She feels terrible for other COVID-19 patients, or their survivors, who are facing similar financial hardships, adding “that’s another part of this (COVID-19 story) that isn’t getting enough attention.”
Brandie and Tim have since read stories about ICU units that became filled to capacity, forcing doctors and nurses to treat five or more critical care COVID-19 patients simultaneously.
“Every doctor and nurse in that CICU unit was involved (in Timmy’s care),” she notes. “If Timmy went into a hospital today, there’s no way he would have received all of this attention …. I doubt he’d be here today.”
For his part, Tim McCain says his near-death experience has given him a new philosophy on life.
“The Good Lord left me on this earth for some reason, and now I need to find out what it is. “Who knows? This (telling my story) might be it,” he says, adding, “this thing almost killed me. I’m going to live every day like it is my last. I don’t want to miss out on anything. That’s the way I look at life now.”
Bill Rice, Jr. is a freelance writer in Troy, Alabama. He can be reached by email at:
wjricejunior@gmail.com


