By Guest Contributor Douglas McKenzie, PhD
Douglas McKenzie. PhD is semi-retired immunologist/molecular biologist who spent twenty-plus years in the biotech/pharma industry inventing and developing novel molecular diagnostics and therapeutics.
April 16, 2020
- An explanation for the everyman
- The solution involves precision containment and treatment of the short-distance social groups which serve as virus reservoirs
- The solution does not require a vaccine
- A rebuttal to Emmanuel’s insistence on long-term imposition of social distancing and the need for a vaccine
Introduction
I keep asking myself what are the possible metrics for the COVID-19 pandemic which will allow us to resume our normal lives, how will we know when it’s time?
Since early March, citizens across our country have been subjected to increasingly stringent limitations on their social interactions, put in place through edicts originating with state governors. The stated purpose of these directives was to control the rate of expansion in subjects infected with the SARS-CoV-2 virus. I don’t need to describe the effects this has had, involving wholesale disruption of the American social fabric and its vibrant economy. I can’t think of a single person who relishes this sort of life, though I do question the motives of some in Washington DC about whether their primary interest is to end the pandemic or use it to implement some new political agenda. I abhor how so-called experts have used faulty models to create harmful public policy which destabilizes our country.
Flattening the curve
On March 15, 2020 President Trump and the Coronavirus Task Force introduced a 15-day period of national vigilance, calling citizens to focus on social distancing. Through analysis of the data around this period and up to the present, it is evident that the nation responded. I want to examine the scientific implications of this effort.
Prior to the vigilance, the daily growth rate for the entire country, the state of New York, and California had been 31%, 36%, and 24%, respectively (see Figure 1). Notice that the spike in new cases in NY was of such a magnitude that it was reflected in the national growth rate for new cases.
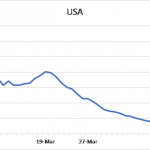


Figure 1: 5-day moving average of daily growth rates for new confirmed SARS-CoV-2 virus infections over time in the entire USA, New York, and California
Of interest is what has happened around the end of 15-day vigilance period. March 27 stands out as a pivotal point for both the USA and New York, because a sizable shift was noted for both. Note how both curves drop rapidly and then transition into a slower phase of decline. California underwent the same pattern of change although the transition on March 27th was not so apparent from the figure. Other states (not shown) also followed a similar pattern of gradual decline in the daily growth rate of new cases. This decline persists to this day across the nation. The three figures show results up to and including April 14th.
Changes of this magnitude (> greater than 20%) were certainly enough to alter the trajectory of the COVID-19 pandemic away from the 1 million cases that would have happened around April 2, and more importantly, to “flatten the curve” in order avoid the projected overloading of our hospitals and their intensive care units.
What does the future portend?
In order to encourage adherence by citizens with the guidelines, figures were widely circulated showing how “flattening the curve” worked. Figure 2 shows the one from the CDC. What these indicate is that curve flattening would not alter the number of infections due to the SARS-CoV-2 virus, it would simply spread them out over a longer period. The model had two important implications; first, slowing the virus via curve flattening had nothing to do with stopping the pandemic, and second, because of curve flattening it was asserted that SARS-CoV-2 would be with us for a long time.

Figure 2: A typical curve demonstrating how curve flattening was thought to work
While Dr. Birx has been emphatic on the use of a logarithmic scale for looking at the curve flattening data, I decided to focus on a different output, namely, the 5-day moving average for daily new cases plotted against time. Using this averaging method allows for better visualization of the underlying patterns. I used this approach to look at new cases emanating from different sources. Figure 3 presents the results for the entire country, New York, and California, starting at a time just before the 15-day vigilance period, and ending at April 19. Each panel demonstrates a similar pattern, namely, curves reaching a maximum rate of decline and then transitioning to a slower phase where there is a fairly consistent generation of new cases. The eventual course of the later phase requires further development before its meaning become totally clear, but it is possible that this reflects the new case load as predicted by curve flattening in Figure 2.

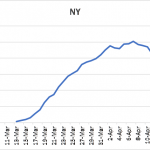
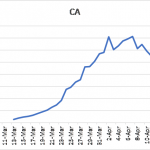 Figure 3: 5-day moving average of daily number of new, confirmed SARS-CoV-2 virus infections in for the entire country, New York, and California
Figure 3: 5-day moving average of daily number of new, confirmed SARS-CoV-2 virus infections in for the entire country, New York, and California
Analysis of new cases really gets really interesting when you look at other states. Some states, like Massachusetts and Georgia have not undergone the same type of curve maximum as New York or California (see Figure 4 left panel). Their growth curves for new cases appear to still be on the ascendancy, suggesting that SARS-CoV-2 virus continues to expand there. At the other end of the scale are states like Florida, Louisiana, and Washington (see Figure 4 center and right panels). Each of these states has experienced a peak in cases, but unlike New York or California they are clearly positioned to minimize new cases either now or in the future. Washington state stands out in this regard: the 5-day moving average of daily new cases is at 200 cases as of this writing.

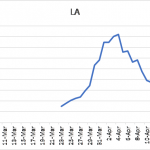
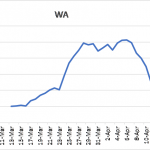
Figure 4. 5-day moving average of daily number of new, confirmed SARS-CoV-2 virus infections in for Massachusetts (MA), Louisiana (LA), Washington state (WA).
This leads to an intriguing observation. If one compares the growth rates of new cases in each state to the growth in the number of daily new cases, one thing stands out. There is a clear association between the pattern of new cases in a state, whether they have peaked and if so, what is their current trajectory? Are they positioned on a plateau or on an ascendancy towards a case-load minimum, with the 5-day moving average for growth rate of new cases. The data for this is shown in Table 1. The metrics for the entire country is in the middle of the table. In Washington state, the apparent fast decline in new cases is related to the fact that this state has the slowest rate of new case expansion. At the other end of the spectrum, the continued expansions of SARS-CoV-2 virus infections in Georgia appears to be related to fact that their growth rate for new cases is the highest among the states which we examined; they have yet to reach their maximum in numbers of new cases.

Table 1: Comparison of growth rates in new SARS-CoV-2 with the patterns of SARS-CoV-2 case load over time. Daily growth rate is 5-day rolling average as of April 16, 2020.
I believe there several important implications to this data.
First, Figure 1 suggests that social distancing appears to have reached a point of diminishing returns. With each passing day it is getting harder to extract meaningful drops in the growth rate. One can project a time when rates are likely to be <2% for the entire country, but that involves wishful thinking. The better question is how you speed this process, driving the effective elimination of virus reservoirs that are needed for perpetuation of infections.
Second, depending on differences in the growth rate for new cases, the outcomes may be quite different. If growth rates persist at levels above 4%, then it is possible that the daily addition of new cases loads will remain quite constant, like what is shown in Figure 3, and fulfilling the implications described for curve flattening. By contrast, if growth rates can be decreased to <2% then the likelihood for virus transmission drops to levels below what is needed for effective transmission and creation of new cases, effectively extinguishing virus reservoirs and terminating the pandemic.
Third, while social distancing was never intended to eliminate infections, perhaps unexpectedly it has brought to a point where the number of new cases are of a magnitude where they are manageable from a containment and treatment prospective.
Fourth, the degree to which social distancing has been effective may be different for different locales. I would argue that population density might be a critical factor, creating conditions favoring the extensive human interactions required for viral transmission which do not exist in less dense settings. In other words, there are risk factors associated with geographical and demographic differences. Any containment and treatment protocol should be adaptable to the conditions under which it is used.
Overall, the real data impacts how we should move forward in monitoring and treating SARS-CoV-2 infections to ensure complete and effective elimination of viral reservoirs so at to prevent reemergence as well as helping us formulate a plan to help people resume their normal lives.
A rational plan for triaging subjects in a post-social distancing era is discussed in the next section.
Identification and Characterization of the Problem
The point of this article is to provide a containment and treatment strategy for ensuring the elimination of SARS-CoV-2 reservoirs, one which would provide the metrics needed for guiding resumption of our normal lives.
The local setting helps puts things in prospective
I live in San Diego, so I’m going to use conditions here to make a point. It helps for clarity to consider the COVID-19 pandemic from a local perspective. People can relate to familiar environments. If you’re not in San Diego, chances are that your local situation is fairly like mine.
As of April 2, 2020, there were 849 confirmed cases of SARS-CoV-2 in San Diego, and we have a population of roughly 3.3 million residents (we are basically stable at this population level). That means that there were currently 1 confirmed SARS-CoV-2 case per 3,887 residents, or 0.025% of the population was infected. San Diego county consists of 4526 square miles, or approximately a single case of SARS-CoV-2 for every square mile. The numbers have increased since I began writing this, but the message is still the same.
If you create a map reflecting the situation, it involves SARS-CoV-2 hot-spots dispersed over a broad area. Consider what that means; from a transmission standpoint, the chances of running into a person infected with SARS-CoV-2 on a simple random walk-about is quite small. Beyond its potential implications for viral transmission, the mapping has important information affecting how we effectively “contain and treat” SARS-CoV-2 for the purpose of ending the pandemic.
For an additional point of reference, even under the worst-case scenario the recent Stanford study looking at detection of virus-specific antibody, suggests that only 4.2% of the residents have experienced an infection event with SARS-CoV-2.
Relative risks in the community setting
At the outset of the SARS-CoV-2 pandemic it was firmly established that transmission of the virus typically involved extensive contact with family members, because they fulfilled the requirement for prolonged exposure. Chance or short-term encounters were less likely to result in transmission of the virus. In recognition of this, the CDC issued a guidance identifying four levels of risk for healthcare personnel based on their exposure (involving both closeness and duration of contact), and their use of personal protective equipment (PPE) during interactions with SARS-CoV-2 infected persons. Adherence to these guidelines has largely protected hospital personnel against infection. The CDC has also issued community level guidelines which are similar in content, but which only consist of two categories: you are either at risk from extended unprotected exposure or you aren’t.
I argue that based on the distribution of cases (i.e. hotspots) among the general populace, as described above for San Diego, that there is a pressing need to focus on identifying persons whose high relative risk could be a factor in the persistence of SARS-CoV-2 infections. In the case of cities, like New York City, the population density alone may artificially serve to drive the creation of “hot-spots”.
The Solution
Need for rational triage method combining testing and treatment of new cases and their short distance social contacts
To move forward towards ending this pandemic requires the use of a rational triage method which combines highly specific containment and treatment. The justification for this approach is that transmission is not random, that it involves transfer of virus between individuals at a short social distance, and that these interactions are knowable and predictable. Like it or not, they continue to exist even in the face of social distancing. We can treat them and prevent their further spread of virus, stopping the pandemic. It involves a precision akin to today’s guided missiles which directly target our enemies with minimal collateral damage to those around them.
Containment
The containment phase should consist of a focused effort to identify individuals who are infected with SARS-CoV-2 (i.e., those persons who are viral reservoirs), and then proactively seek all persons who are within a short social distance from them, including family members, roommates, friends, co-workers, etc. (i.e., persons who are at the highest risk). Epidemiologists would call this surveillance and contact tracing, something they did at the very outset of the pandemic for a few cases but which is not widely practiced at present. Contact tracing has played a major role in communicable disease control, most notably smallpox. These persons are then tested, in an ever widening the search for “at risk” individuals, until there is evidence that the transmission hot spot has been completely identified.
Subjects would be tested both prior to therapy and again 5-7 days after therapy (see below). The testing would consist of both PCR-based testing for SARS-CoV-2 as an indicator of infection and serological testing for the presence of virus-specific IgG/IgM as a measure of immunity. It is noteworthy that this sort of dual profiling, while primarily pin-pointing people at risk for new infections, would also identify asymptomatic infected individuals who could account for the infection of the initial subject whose test result started the hot-spot search and profiling. With more experience, the profiling would lead to the generation of risk factors for certain types of contacts, helping ensure that all potentially relevant persons are screened.
Using analytics applied to treated persons, you would be able to quantitatively establish the elimination of viral reservoirs. This would form the basis of the metrics for knowing that the pandemic was over, or at least contained to a point where there were exceedingly small reservoirs of virus and carriers to perpetuate its expansion.
Analysis of the antibody response would contribute to understanding what role immunity played in controlling the spread of virus. There is presently a lot of speculating about what immunity means, but we don’t yet have enough data to know.
Testing driving treatment at the early stages of infection
SARS-CoV-2 testing is increasingly rapid. In one example involving a local hospital that I know of, the turn-around time has been reduced to around one hour. The point is not to suggest that all testing is fast, but rather to underscore that with the necessary effort, testing need not be a limiting factor.
Justification for the use of hydroxychloroquine and azithromycin in treatment
Any viral infection involves a battle between two opposing forces, the invading pathogen and host’s innate immune system. The virus enters host cells and begins replicating, thereby increasing its numbers and capacity for winning the struggle. Meanwhile the host counters by calling upon its innate immunity, an ancient system which evolved to repel viral and bacterial challenges. Hydroxychloroquine (HC) stops the virus’s capacity to replicate in the cell, blocking an essential step in the spread of the virus. There is no way around this step, and it cannot be circumvented by mutation. Azithromycin (AZ) supplements the activity of hydroxychloroquine by protecting the innate immunity signaling from SARS-CoV-2’s effort to turn it off; that’s the basis of azithromycin’s anti-viral activity which is different from how the drug works on bacteria. Thus, the drugs work by shifting the balance of power back towards the host.
The degree to which the host remains capable of repelling the virus is linked to their clinical status. This explains why HC by itself works extremely well early in the infections, when viral loads are limited and symptoms may be present, but the situation is not yet overwhelming. The addition of AZ allows for the combination to be even more effective in treating patients further into the infection, including when persons are hospitalized. Where the drug combination doesn’t work, is when the infection has advanced too far, as we see in patients who are already intubated before drug treatment has begun. In these advanced stage patients, the “walls of the castle” have been breached, and the invaders have overrun the castle. Alternatively, HC is not indicated for use in subjects with SARS-CoV-2 co-morbidities. If you hear Dr. Fauci saying HC doesn’t work in all cases, understand that he is being disingenuous at best. The drug and its combination work extremely well in all cases where innate immunity still has the capacity, if properly augmented, to clear the SARS-CoV-2 infection. I have a paper in preparation which I think will contribute to the dialog on this. It explains the mechanisms of HC and AZ and why they are so effective in clearing SARS-CoV-2 infections.
Treatments involve therapeutic and prophylactic treatments depending on risk analysis
As for treatment with HC or AZ, it could be done in two different but related manners. A subject who tests positive for SARS-CoV-2 would be immediately put on a 5-7 course of HC. Standard dosing regimens would be used. Alternatively, prophylactic treatment with HC could be instituted even before the test results are in. As mentioned above, the data suggests that HC is most effective when viral loads are limited, so prophylactic HC would be justified. This is what proved effective in the treatment of Michigan State Legislative Representative Karen Whitsett, such that she now credits HC with saving her life. The addition of AZ to the therapy would be left to the doctor’s discretion.
Clearly, if HC eliminates viral load in 4-5 days, it is cutting into the time and likelihood that a SARS-CoV-2 infected individual could transmit the infection to someone else. At the current national growth rate of 4.24%, a single individual would successfully transmit the virus only once every 17 days, meaning HC therapy would prevent successful viral transmission.
Unless the individual harbors any co-morbidities, they would be sent home after receiving HC/AZ and asked to return for retesting 5-7 days later. Whether the individuals within the short social distance are treated with drug(s) is dependent on their wishes and advice from their doctor. If it were me, and I knew my risk of infection was elevated by virtue of my interaction with a SARS-CoV-2 infected individual, I would give serious consideration to prophylactic HC treatment. The drug is both safe and effective under the conditions discussed here. There is no discounting this despite what some are distorting in the news. The idea to use HC to treat coronavirus was first suggested back in 2003 (Savarino et al., Lancet Infect Dis. 2003 Nov;3(11):722-7).
Extinguishing hot spots of viral infection
In any case, the treatment with HC prevents disease progression, so coupling it with virus testing is an effective contain and treatment paradigm. And again, by repeating this across the subjects within a short social distance ensures that the viral hot spot will be extinguished. Every new case of SAR infection should be considered a new hot spot.
This program can be implemented in short order. All it would require is conveyance of the details to healthcare providers that they treat incoming subjects in a new triage method as described herein. Presently, here in San Diego, all potential new cases of SARS-CoV-2 infection are already triaged through their local physician. All that would change is the expansion of the testing involved, the recognition that HC plus or minus AZ is to be administered to all newly confirmed SARS-CoV-2 subjects, and that their short social distant contacts need to be contacted and put into the containment and treatment queue.
How can we know whether the proposed triage method would work?
Epidemiology units in the local public health agencies could easily and swiftly establish proof-of-concept if needed. There is an adequate base of new SARS-CoV-2 cases, and the current standard of care doesn’t involve any therapeutic intervention. It would be a simple matter of enrolling subjects in a clinical trial where a treatment group was administered HC following confirmation of a SARS-CoV-2 infection, and “viral load” determined in both the control and the treated group 5-7 days later. The primary outcome would address whether HC administration led to a statistically significant reduction in viral load. Other secondary outcomes, which other clinicians say are improved by HC, might include a reduction in fever, a reduction in need for hospitalization, and the acquisition of immunity. The results from this trial could be available within two weeks if the trial were started today.
Role of the epidemiology units from local public health agencies in the new triage scheme
I already described above how epidemiology units need to address fundamental aspects of viral transmission which occurs while social distancing edicts are in place. In the new triage protocol, these units would take on added responsibility, assuming the function of identifying, contacting, and following up with the short social distance contacts of all new SARS-CoV-2 cases. I don’t think this needs to be onerous or involve any invasion of privacy or loss of personal freedoms. In effect, their work would ensure individuals at elevated risk for new infections get tested and at a minimum, are allowed access to prophylactic HC (see above and AZ).
Integrating risk factors and social media into their daily functions might forever alter the nature of the work conducted by local epidemiology units. They could be the means by which the public learns information about the levels of residual viral reservoirs which exist in their region. I didn’t touch on the potential social media tools they might use in this task. Clearly, there have been many ingenious answers proposed recently for interrogating how a person’s interactions might contribute to virus transmission; for example, see MIT’s new app which looks to use individuals' smartphones as tools for automatic COVID-19 contact tracing.
Metrics for resumption of normal life
I have argued that the proposed triage method could be the basis of metrics used for returning to work. I think that establishing the number of new SARS-CoV-2 infections daily could serve as the primary determinant in whether normal life should be resumed. Other metrics such as the number of persons with SARS-CoV-2 infections being admitted to the hospital on a daily basis, the number of SARS-CoV-2 cases being treated with HC, and the percentage which are responding, are other possible metrics by which we could base the decision to resume normal life. People would welcome hard evidence to make personal decisions. Governors and government agencies would too.
What Others Suggest
Space doesn’t allow me to thoroughly address alternative plans advanced by others for facilitating the return to normal life. What I do wish to address is the call for the development of a SARS-CoV-2 vaccine, and its use in treating ongoing infections. Some have argued that its administration should be a condition for ending the pandemic and returning to a normal existence. This is perhaps the most ill-advised therapeutic proposal that I have ever seen. That it would be given serious consideration for treating an ongoing pandemic is preposterous.
Right off, the duration of the project is disqualifying. The development and approval of a vaccine takes a minimum of 4-5 years, and that is just to make it through the rigors of standard development under the best of circumstances.
In addition, the rate of failure in vaccine development is high. You shouldn’t trust anybody who says they can do it faster, or they already possess the needed know-how. Drug or vaccine development programs ALWAYS hit snags, and that adds unanticipated time to their development. I suspect that in the period needed for development, and at its current rate of expansion, the SARS-CoV-2 infection would have spread throughout the world’s entire population by project’s end, before the vaccine was ever administered to a single subject.
This is before we even touch upon the potential issues of safety and efficacy. We do know that similar programs involving past pathogens have not resulted in any other approved vaccines but for a single exception- Merck’s Ebola vaccine. The 2003 SARS pandemic was greeted with a similar call for vaccines, and as of now, no SARS vaccines have been approved for use in man. One group spoke of what I envisioned above; by the time their vaccine was ready for testing there was no longer a need as the pandemic had passed. And speak of snags, RB Couch of the University of Texas has published articles on how SARS vaccine candidates elicited pulmonary immunopathology in mice on challenge with the SARS virus. These articles point to the fact that we know little about the coronavirus-host relations and how induced immunity might affect normal tissue function. Finally, other studies with SAR vaccine candidates have found that vaccinated animals still display significant disease upon challenge, that is, they didn’t clear the virus. We simply do not know whether SARS-CoV-2 vaccines will be ineffective, or even worse, unsafe. Finally, discussions of vaccine always sound like a single solitary task or path, but there is more to address. Each vaccine comes with considerations about administration, their use in different populations (i.e., children or the aged), and whether they require other agents, like adjuvants, in order to achieve their full potential. Identifying the conditions for use and appropriate populations adds a level of complication which is either overlooked or not understood by those promoting a SARS-CoV-2 vaccine. What worries me is that fear of the SARS-CoV-2 will result in our embracing terrible policy decisions like making a SARS-CoV-2 vaccine.
I have nothing against the development of a vaccine for SARS or SARS-CoV-2, if it’s conducted using standard development paths and timelines, and not while trying to race an advancing pathogen. Vaccine development also requires expertise which I do not see at the NIAID. That is, there is no history of success to give us any comfort that the program will work. I’d like to point out that we’ve been waiting for the HIV vaccine which we were promised since 1984.
It’s somewhat easy for Ezekiel Emanuel, a health policy expert and Vice-Provost of the University of Pennsylvania, to overlook these considerations as he tells us we must stay “locked-down” for 12-18 months until there’s a vaccine. That’s kind of his style - fright merchant. But Dr. Fauci should understand how daunting the task is, and the real duration which is involved. Maybe that’s why he only gives vaccines praise, describing them as a “game changer”, instead of making a hard commitment to their development. The bigger concern is why he is not interested in exploring all options regarding ending the SARS-CoV-2 pandemic. While he may harbor concerns about HC therapy, his lack of interest in conducting short term pivotal studies to ultimately determine their utility in SARS-CoV-2 is highly disconcerting.
Closing Thoughts
Through social distancing a reduction in growth rate of new SARS-CoV-2 has been achieved,putting many localities on the path to the potential control of new cases. In many locales there is a need to supplement the effort with rational containment and treatment methods.
The containment and treatment method proposed here has all the characteristics required for ending the coronavirus lockdowns and a providing a path for resuming our normal lives. It is fast, easy, and cost-effective to implement, data exists which gives proof to the proposed concept, the treatment is short in duration, can be used in children, and involves drugs whose efficacy and safety are well established. It serves to eliminate viral reservoir which are perpetuating the pandemic. It also provides for quantitative measurements of viral presence that can be used in determining that it is safe to resume our normal lives. The containment portion is consistent with plans advanced on April 14 by Admiral Brett Giroir, the assistant Secretary for Health. It is time to explore the validation and the implementation of this solution.
Douglas McKenzie. PhD is semi-retired immunologist/molecular biologist who spent twenty-plus years in the biotech/pharma industry inventing and developing novel molecular diagnostics and therapeutics. Now he spends his time constructing comprehensive disease frameworks for cancer drug resistance/disease relapse and Alzheimer’s disease for the purpose of identifying new therapeutic approaches and drug candidates which can be accelerated into the clinic. The article reflects his interest in providing solutions which can hasten the end of COVID-19 pandemic. He is currently writing a scientific article detailing mechanisms of actions for hydroxychloroquine and azithromycin and how they synergize in treatment of SAR-CoV2 infections, information which is absent from the dialog about therapeutic options.


